Sir Peter Ratcliffe – Nobel Prize / Physiology or Medicine 2019An Anglo /American collaboration shared with William Kaelin and Greg Semenza for their work on hypoxia
I had the privilege of interviewing Sir Peter Ratcliffe at the Francis Crick Institute in January 2020. He had recently returned from Stockholm after receiving, probably the most coveted of awards, The Nobel Prize, for his work on hypoxia. He was keen to acknowledge the work was a collaborative effort with his two American Colleagues, William Kaelin and Greg Semenza together with his dedicated teams in both Oxford and the Crick.
Nurses are very aware of potentially hypoxic situations. Monitoring blood oxygen levels is part of normal day to day patient observation. But do we ever really think about oxygen in a meaningful way, the oxygen in the air we breathe to the oxygen we administer therapeutically. It has been known for over a century that at high altitude, with a lowering of atmospheric pressure, blood oxygen levels fall. This is why mountaineers climbing the highest peaks in Nepal, spend time at ‘base camp’ to become acclimatised — in reality the biochemical processes take over as more red blood cells are produced to transport oxygen. The reverse occurs at low altitude with a higher atmospheric pressure. Those with reduced respiratory function suffering from diseases such as cystic fibrosis, find a visit to the dead sea, which is below sea level, beneficial as their breathing becomes less laboured.
The English chemist, Joseph Priestly isolated oxygen in 1774, although he called it dephlogisticated air. At around the same time, another scientist, Joseph Black of the University of Glasgow, discovered carbon dioxide. It was not until a century later, John Scott Haldane, a graduate of Edinburgh medical School, examined in more detail these two gases. He understood the consequences of oxygen lack but also found it was a high blood carbon dioxide level to be the main trigger controlling breathing. Haldane discovered that a lack of oxygen did not increase the breathing rate, it was the rapid increase in the pulse rate and output of blood from the heart that allowed organs to receive a greater flow of blood to compensate for the lack of oxygen. Ratcliffe talked of his early heroine, Mabel Fitzgerald, who in 1911 accompanied Haldane to Pikes Peak in Colorado, where they began to investigate human respiration at high altitudes. She was the only woman to accompany this expedition and her detailed recordings and observations of full altitude acclimatization on carbon dioxide tension and haemoglobin are standard today. As a woman in the early 1900’s it was difficult for her to study or be recognised by the Royal Society as with Universities, these were male dominated institutions, which makes her achievements all the more incredible. (1)
In more recent times, Ratcliffe , building on this early work, established a laboratory in Oxford University’s Nuffield Department to explore the regulation of erythropoietin ( EPO) a hormone released by the kidneys in response to low oxygen levels. EPO, by stimulating the bone marrow, is responsible for the production of red blood cells. Nurses working in renal units will be familiar with Aranesp Injections used to treat symptomatic anaemia associated with chronic renal failure. Synthetic EPO was first used successfully to treat anaemia in 1987 (2) When the kidney is compromised and unable to produce enough natural EPO hormone, the bone marrow is unable to manufacture sufficient red blood cells. This physiological response has been known for some time but what Ratcliffe sought to explore was how cells sense and respond to oxygen depletion leading to EPO production. Much to his surprise he discovered that it was not only the kidneys that had this ability, but also the spleen, brain, skin and testes. He found that mRNA (the messenger from DNA) was present in all cells, but the kidney was particularly sensitive to oxygen depletion. He suspected that the kidney may be an early trigger as the blood supply to the kidney is unique and unusual in its formation. At the junction between the renal cortex and the renal medulla, the interlobar arteries form the arcuate arteries, turn to follow the contours of the renal pyramids and a hypothesis is suggestive this may interfere with oxygenation as the arteries in effect turn back on themselves. However, finding that cells from other organs could also stimulate EPO production when deprived of oxygen was truly revelatory and he wanted to examine the molecular pathway which enabled cells to detect hypoxia and turn on EPA production.
Finding that the binding of proteins expressed by the VonHippel-Landau tumour suppressor gene ( VHL) to hypoxia -inducible factors ( HIF), a transcription factor which trans-activates the EPO gene, was a breakthrough. HIF transcriptional complex had been discovered by Greg Semenza in 1995.(3)
When oxygen levels fall VHL does not bind HIF allowing it to activate the EPO gene. The body completes this process at an amazing speed once hypoxia occurs. Ratcliffe is justifiably proud and hopes that the research will lead into the development of new drugs which will assist the body in this process.
After completing his medical degree at Cambridge, he specialised in renal medicine and continued to work as a senior Consultant Nephrologist for many years, eventually splitting his clinical work with the scientific. The motto at the Francis Crick Institute, is ‘Discovery without boundaries’, Ratcliffe maintains however unfashionable a research subject, as hypoxia was in the early 1990’s , there is always more to learn. If unravelling the chain of events that all cells use to sense hypoxia, may in some way produce improved outcomes for patients then no effort is ever wasted. (4)
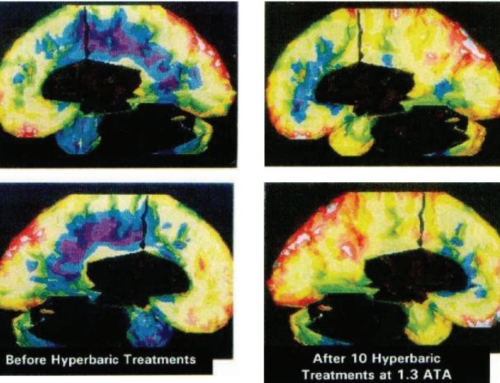
Hyperbaric oxygenation is the most efficient way to help ameliorate symptoms of hypoxia.
© Jane Dean
References
- Fitzgerald MP; 1913 The changes in the breathing and the blood at various high altitudes; Philosophical Transactions of the Royal Society of London. Series B 203 ( 294-302) : 352-371
- Eschbach JW, Egrie JC, Downing MR, Browne JK, Adamson JW; 1987
- Correction of the anaemia of end-stage renal disease with recombinant human erythropoietin. Results of a combined phase 1 and 2 critical trial. The New England Journal of Medicine 316 (2) 73-78
- Wang GL, Semenza GL, 1995 Purification and characterization of hypoxia-inducible factor 1. The Journal of Biological Chemistry. 270 (3) 1230-7
- Ratcliffe P, Semenza, G, Kaelin W. 2019 The Nobel Prize in Physiology or Medicine. Nobel Prize.org
Jane Dean MA Health Research.
Freelance Health Writer and Author.
Founder of A Breath for Life Children’s Charity and Hyperbaric Oxygen Facility