 Oxygen Treatment for Children with Autism Philip B James. Emeritus Professor of Medicine, University of Dundee.
Oxygen Treatment for Children with Autism Philip B James. Emeritus Professor of Medicine, University of Dundee.
Until the 1990s few children were labelled as ‘autistic’ and it is clear that the recent epidemic is not because of better diagnosis, it is because some aspect of the medical management of children at birth or in early childhood has changed.
The blood vessels of the brain are different to those in the rest of the body; they form a barrier because many substances present in blood are toxic. The barrier, known as the blood-brain barrier or ‘BBB’ needs energy to work properly and so is particularly affected by hypoxia, that is, lack of oxygen. Brain damage due to failure of the BBB can occur at any time during life but especially, as MRI has shown, at birth. After an initial insult the barrier may remain damaged as it does, for example, in many multiple sclerosis patients.
The use of oxygen in medical practice lags well behind the latest research findings of biological scientists indicating its central importance in healing. Oxygen is simply regarded as necessary for the production of energy and is given as a supplement to ensure that blood is red. However, it has been shown that oxygen levels control the expression of many genes including those responsible for new blood vessel formation, the control of inflammation and the release of stem cells into the circulation. These processes are critical to the repair of all tissues, but especially the brain. Breathing is not only essential to gain oxygen for normal function, but also for recovery from injury or illness. Unfortunately, injury and disease often damage blood vessels and this restricts the delivery of oxygen just when it is most needed for repair.
Misunderstandings about the toxicity of oxygen have generally clouded judgement about the use of high levels in treatment, but enormous experience exists outside mainstream medicine from aviation, space and underwater medicine which has demonstrated the extreme safety of using high levels of oxygen in treatment. To significantly increase the level of oxygen carried in the blood needs a pressure chamber and it is well-established, if not well-known, that giving a high level of oxygen for just one hour a day may promote the repair of tissues when all other medical interventions have failed. In other words giving more oxygen extends the envelope of natural recovery. There is no substitute for oxygen and if giving more does not help a patient it is not because oxygen does not ‘work’ it is because the damage has gone too far to allow normal recovery.
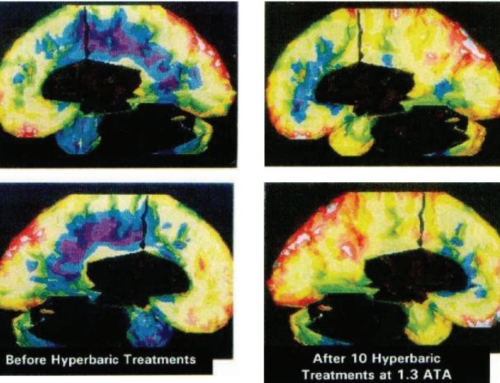
However, key questions are the dosage of oxygen needed and the number of treatment sessions for a given patient. The original studies of hyperbaric oxygen treatment for multiple sclerosis sufferers used a course of 20 sessions and this number was also used for the controlled studies. Over the last 27 years the UK charity centres have also used an initial course of 20 sessions, titrating the dose based on the patient’s response, followed by weekly maintenance sessions because multiple sclerosis is often a progressive illness. A course of 20 sessions on a daily basis for five days a week means that a course can be completed in a month. The evidence supports using oxygen by hood at 1.5 ata, or 1.75 ata using a mask for optimum results. However, significant benefit has been reported in a double-blind controlled trial in autistic children from 40 sessions at a pressure as low as 1.3 ata with 24% oxygen. This pressure, which can easily be achieved using commercial jet aircraft pressurised on the ground, is also highly effective in treating acute mountain sickness affecting the lungs and the brain.