Diabetes Update
DIABETIC CARE, IS HYPERBARIC OXYGEN A VIABLE TREATMENT OPTION?
Recent Cochrane reviews show no positive evidence for incorporating hyperbaric oxygen treatment (HBOT) for diabetic neuropathy. There is no evidence of any adverse effects, simply more research is needed to obtain any conclusive data. Most of the trials are non randomised with methodological limitations and are therefore a poor source of evidence, however the consistency of positive results is noteworthy.
The National Institute of Clinical Excellence ( NICE) only recommend HBOT for certain conditions primarily decompression sickness. The chairman of NICE, Sir Michael Rawlings has argued that recognition should be given to observational studies, which would include those produced by practitioners of HBOT.
As a result of these guidelines, many Physicians are reluctant to prescribe a course of HBOT for their patients and as there are so few hyperbaric chambers in a clinical setting, Physicians are unable to gain experience of HBOT to make their own informed decisions.
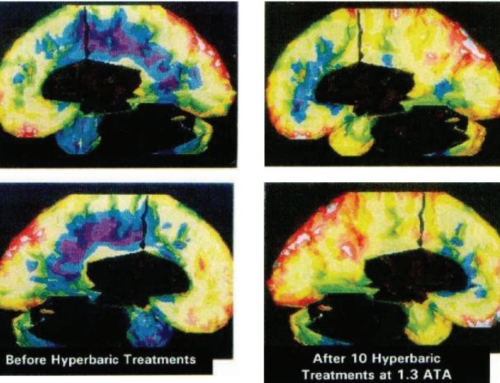
Anecdotal evidence is insufficient to convince even the most forward thinking Physician, however to a lay person, anecdotal evidence with some visual photographic proof, is often sufficient to convince them to self refer. With changing attitudes, many patients research available options when frustrated with limited improvement from conventional treatments.
This is the position at the charity chamber run by A Breath for Life, where almost all patients self refer. This is not for profit establishment, unlike America where HBOT is big business. A Breath for Life patients are asked to donate £20 for an adult and £10 for a child. The charity would never turn away a child in need, so donations are not always sought. Minimum cost in a USA chamber would be $300 and often much higher, up to $1400 in some centres.
It is hard to believe there are 61 non profit chambers, operated by volunteers in the United Kingdom. The majority are charity chambers specialising in the care of patients with multiple sclerosis, although true to say, many of these centres treat a variety of conditions including diabetic neuropathy and foot ulcers. Figures from the hyperbaric oxygen therapy trust (1) suggest 3 million HBOT sessions are carried out each year, without serious side effects or unwanted consequences.
There are some contra-indications for HBOT, pneumothorax, sinus pain, claustrophobia, ruptured ear drum. When treating Type 1 diabetic patients there is a risk of hypoglycaemia if the patient has not had food after their normal insulin dose. The Hyperbaric Medicine Practice text book, states “Of all the medical treatments carried out in hospitals, hyperbaric oxygen treatment is one of the most benign when it comes to side effects”(2)
Chambers are either multi or monoplace. In the UK we also classify chambers,
Types 1 and Type 2 are situated in hospital units providing a high standard of life support capability for acute patients with on site medically qualified staff and certified technicians.
There are 17 such chambers registered with the British Hyperbaric Association.
The chamber at A Breath for Life is a Type 3, purpose built to accommodate 8 persons. Type 3 chambers were once inspected by the Healthcare Commission but were deregulated by an Act of Parliament in 2008, since perceived risks due to fire, oxygen toxicity and infection control proved to be groundless. Oxygen is supplied via valve settings delivered to each individual seat.
The patients primarily self refer after they have investigated available treatments for diabetic neuropathy and leg ulcer. Each patient undertook a series of 20 treatments. The chamber was compressed to the equivalent depth of 24 feet, bringing the internal pressure to approx 1.75 atmospheres. All patients used a face mask for the delivery of oxygen.
The numbers are small, two patients with long standing infected varicose ulcers which were unresponsive to antibiotic treatment; one patient with Charcot’s foot and three patients with sensory neuropathy with impaired proprioception in one or both feet.
Infections were cleared in the varicose ulcer patients and clear signs of healing with granulation apparent in both patients. The Charcot’s foot patient said she felt her feet touch the floor when getting out of bed after the first treatment, which was quite remarkable and after 20 treatments her perception to peripheral stimuli was greatly enhanced
15% of people with diabetes will have a foot ulcer at some point in their lives. Diabetic foot ulcers precede more than 80% of amputations in people with diabetes (3) The Breath for Life patients scored one and two on the Wagner classification. Trauma and infection to the feet of diabetic patients is of serious concern both to them and their medical practitioners. (4)
Research from Sweden on 16 non diabetic patients with chronic leg ulcers showed marked improvement in healing after 30 treatment sessions ( 5)
We do know when adequate blood flow is compromised as in diabetes, oxygen cannot reach the underlying tissue to support the natural healing process. No wound can heal without appropriate oxygenation, which makes the diabetic wound more complex. There is no treatment, other than HBOT, that can provide the necessary oxygen. Breathing 100% oxygen under pressure allows dissolution of oxygen into all bodily fluids, including plasma and lymph to restore and enhance the natural healing process. HBOT stimulates the development of new capillary growth and recent research has shown a significant increase in naturally produced stem cells following treatment. (6)
The results from A Breath for Life are not part of a valid research study as the numbers are so small, however even in such a small cohort, results are encouraging and worthy of further controlled trials.
There is limited evidence to support HBOT being more effective in the treatment of diabetic foot ulcers than standard treatment alone, as only small, randomized controlled trials have been published. The most recent study by Londahl et al (7) successfully randomized 37 patients in which the primary outcome was healing of the index wound in the HBOT group.
Conclusion
HBOT is experiencing a resurgence of interest, as antibiotic resistance is reaching crises with Professor Dame Sally Davies, Chief Medical Officer, predicting a return to widespread sepsis as experienced before the introduction of penicillin. Neutrophils, fibroblasts, macrophages and osteoclasts are all dependent upon oxygen to carry out their specific inflammatory or repair functions. The polymicrobial nature of diabetic foot infections make antibiotic therapy difficult and prolonged.
The diabetic foot clinic at King’s College are pioneering the use of Silhouette, a new wound imaging assessment. It would be useful if HBOT could be included as part of a study using Silhouette, to provide, hopefully strong evidence in support of HBOT as an adjunct to conventional treatments.
In further studies, a trial, involving 20 people by the University of Adelaide, Australia is seeking to test the effectiveness of HBOT for people at risk of developing Type 2 diabetes. Preliminary results suggest that sitting in an oxygen chamber can increase the sensitivity to insulin to the same extent as achieved by losing 13% of body weight.
Once a chamber is established, HBOT is the safest, most cost efficient treatment available to the NHS and has no side effects. There should be no problems to access this treatment, only solutions. The first solution is to equip every hospital or medical clinic with a chamber, train operators and educate both medical personnel and patients on the benefits of breathing oxygen under pressure. Patient compliance is paramount to successful outcomes. The treatment is lengthy with a minimum of 20 treatment sessions recommended and each treatment will take an hour and a half each day. For most patients when they experience noticeable results, the time taken becomes negligible when faced with a lifetime of chronic diabetic neuropathologies.
The cost of diabetes ( www.diabetes.org.uk) is of increasing concern to the NHS. Amputations due to complications of diabetes are expensive and when there are estimated to be 100 such amputations every week, HBOT must be included within the multidisciplinary footcare teams established in most major hospitals.
Professor Philip James of Dundee University and A Breath for Life Honorary Medical Director, has said, “Giving more oxygen is not alternative medicine, it is sound science and common sense. There is no substitute for oxygen”.
Professor James’s book, Hyperbaric Medicine, will be available from July 2014.
REFERENCES
- Hyperbaric Oxygen Treatment Trust,Castle Craig Hospital, West Linton, Scotland EH46 7DH
www.hyperbaricoxygentherapy.org.uk
- Kindwall E P, Whilam H T; Hyperbaric Medicine Practice, 3rd Edition
Best Publishing Company
- Reiber G E er al, Causal pathways for incident lower –extremity ulcers in patients with diabetes; Diabetes Care 1999; 22:157-62
- Adams C A, Deitch E, Diabetic Foot Infections. UMD-New Jersey Medical School, Newark USA ( Available on PubMed)
- Hammarlund C, Sundberg T, Hyperbaric Oxygen reduced Size of Chronic Leg Ulcers; A Randomised Double – Blind Study. Past Reconstructive Surg. 1994 Apr, 93 p.829-33.
- Thom, S R , et al, Stem Cell Mobilization by Hyperbaric Oxygen. Am J Physiol Heart Circ Physiol 290: H1378 –H1386 2006.
- Londahl M, et al, Hyperbaric oxygen therapy facilitates healing of chronic foot ulcers in patients with diabetes. Diabetic Care 2010,33:998-1003.
Author, Jane Dean M.A. RN. RM. Hon.Chairman, A Breath for Life Hyperbaric Oxygen Centre, Borrans Lane, Middleton, Morecambe LA3 3JJ
www.abreathforlife.org
Email:- [email protected]
Telephone:- 01524 855422